A healthy 26-year-old male patient, who had orthodontic treatment as an adolescent, was referred. During clinical assessment, class I malocclusion with moderate occlusal wear facets was observed. No mobility was present. Widened ligament spaces were noted at Nos. 14 and 15. Localized gingival inflammation was found in the maxillary left posterior sextant, with bleeding on probing. Generalized probing depths of 2–4 mm were noted, with an isolated 12 mm buccal depth on the direct buccal of No. 14 and grade 2 furcation invasion. An isolated 5–6 mm probing depth on the distal of No. 14 with grade 1 furcation invasion was also present, along with 2 mm of facial recession. Pulpal vitality testing showed normal cold response and slight percussion response, confirmed by an endodontist. The diagnosis was localized stage 3 grade B periodontitis, or severe chronic periodontitis with bruxism, trauma from occlusion, and normal pulp accompanied by symptomatic apical periodontitis. The minimally invasive, multi-step LANAP® protocol was performed using the PerioLase® MVP-7™ pulsed Nd:YAG laser (Millennium Dental Technologies, Inc., lanap.com). The patient reported minimal discomfort and returned to normal activities the following day. Radiographic imaging at 6 and 12 months post-treatment showed continual improvement in bone fill, reduced gingival inflammation, better tissue quality, and improved clinical probing depth of tooth No. 14.
KEY TAKEAWAYS
Multiple etiologies may contribute to periodontal destruction and disease progression, especially in cases with advanced furcation bone loss. Accurate diagnosis that rules out endodontic involvement is a critical component of a comprehensive assessment.
Trauma from malocclusion can exacerbate the progression of periodontal disease.
THE LASER-ASSISTED LANAP® PROTOCOL precisely targets diseased tissue while occlusal adjustment mitigates further bite trauma, resulting in true regeneration of the attachment apparatus, including new cementum, periodontal ligament, and bone. The LANAP protocol can only be performed using the PerioLase® MVP-7™ free-running pulsed Nd:YAG laser. Its variable pulse durations are particularly suited to control laser-tissue interactions.
Andrew Peterson, DMD, MS
Private Practice, Arcadia, California; Certified Instructor, Institute for Advanced Laser Dentistry

Figure 1
Fig 1 and Fig 2. Extraoral examination revealed slight tenderness in the left TMJ; intraoral examination showed a thin gingival phenotype, localized gingival recession, and loss of clinical attachment. Preoperative buccal (Fig 1) and occlusal (Fig 2) views showed gingival inflammation, minimal recession, and 12-mm probe depth on the direct buccal of tooth No. 14.

Figure 2
Fig 1 and Fig 2. Extraoral examination revealed slight tenderness in the left TMJ; intraoral examination showed a thin gingival phenotype, localized gingival recession, and loss of clinical attachment. Preoperative buccal (Fig 1) and occlusal (Fig 2) views showed gingival inflammation, minimal recession, and 12-mm probe depth on the direct buccal of tooth No. 14.
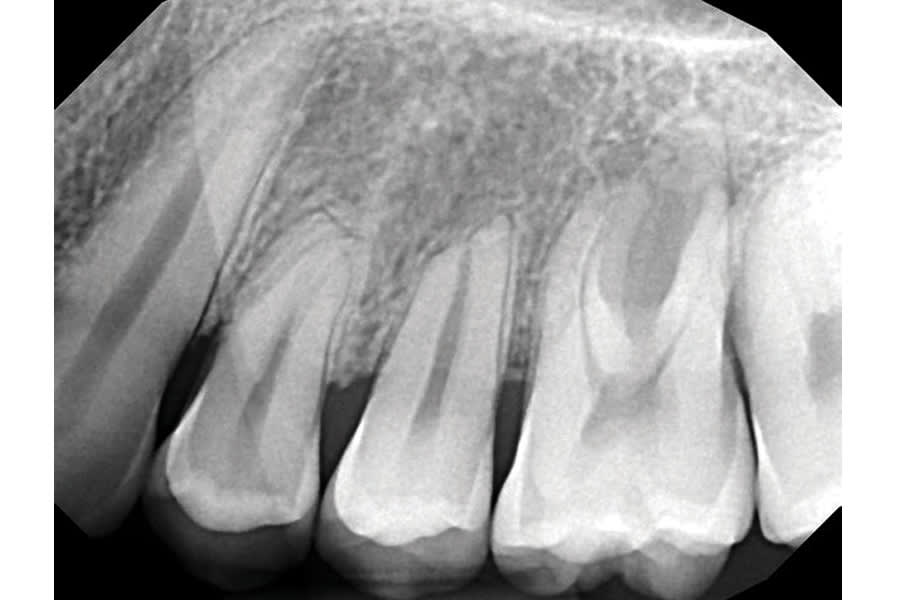
Figure 3
Fig 3. Preoperative periapical radiograph showing short, blunted roots on teeth Nos. 12 through 14, with apical root resorption on No. 13 and the distal buccal root of No. 14. There was close root proximity between Nos. 14 and 15, with moderate interproximal crater formation. Radiographic darkening mainly affected the furcation of No. 14.
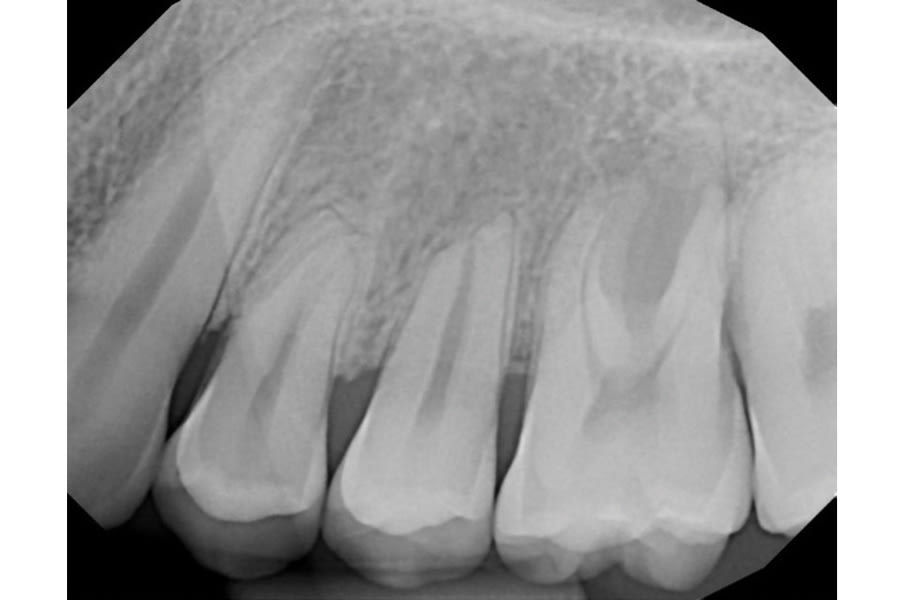
Figure 4
Fig 4. Preoperative CBCT imaging indicating a deep furcation extending to the buccal aspect of the palatal root of No. 14, absence of the buccal plate, and buccal displacement with lingual root torque.
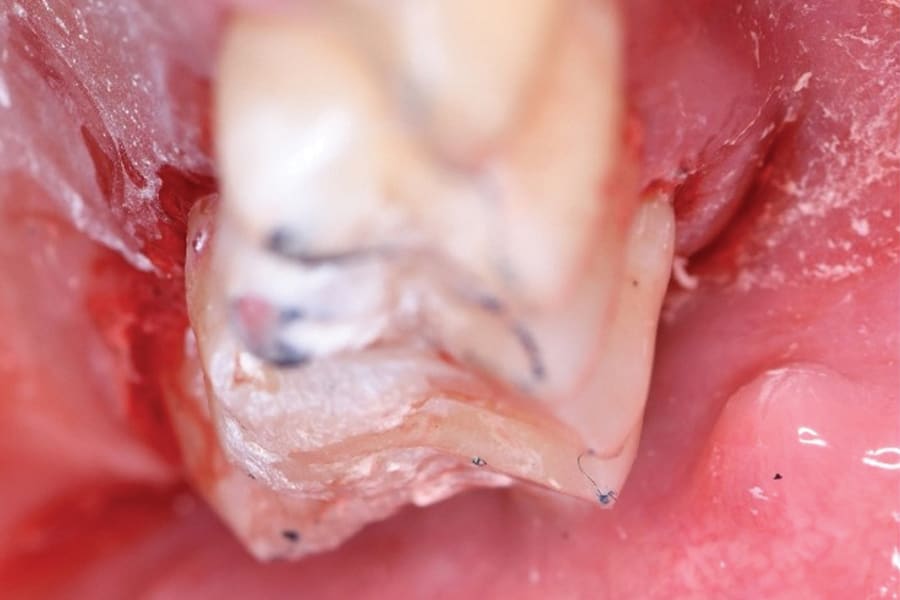
Figure 5
Fig 5. Preoperatively, tooth No. 14 showed steep cusp planes and wear facets.

Figure 6
Fig 6. Occlusal view with heavy adjustment underway as part of the LANAP laser protocol. Localized hemodynamically stable blood clot was present in the sulcus of No. 14. Blunt dissection and bone decortication release the patient’s stem cells. Laser irradiation forms a stable blood clot with live viable cells.
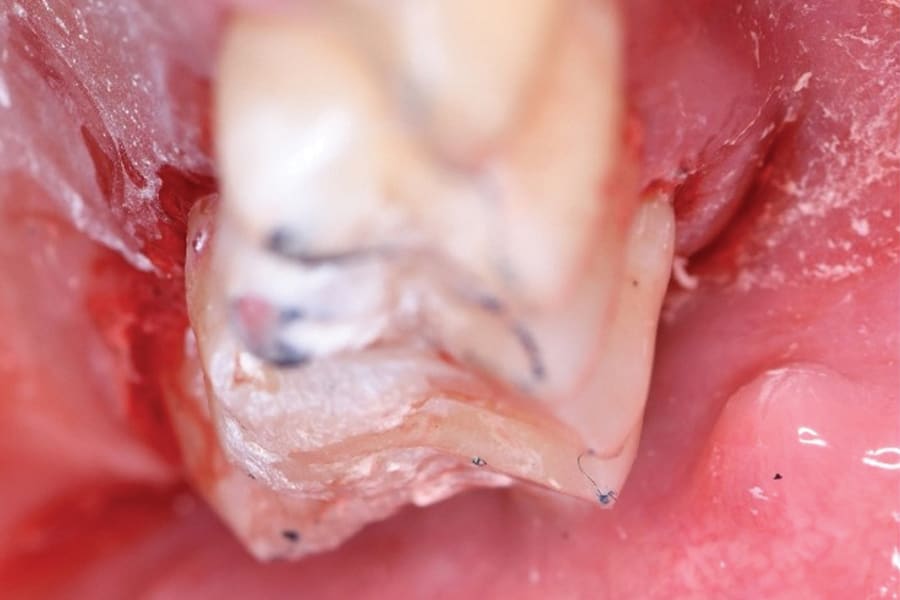
Figure 7
Fig 7. Occlusal view highlights the heavy reduction of the palatal cusp on No. 14.

Figure 8
Fig 8 through Fig 11. Six months after treatment. At 6 months postoperative (Fig 8) there was improved tissue quality and minimal reduction in clinical attachment loss noted by the localized facial recession of 2 mm on the buccal aspect of No. 14.

Figure 9
Fig 8 through Fig 11. Six months after treatment. At 6 months postoperative (Fig 8) there was improved tissue quality and minimal reduction in clinical attachment loss noted by the localized facial recession of 2 mm on the buccal aspect of No. 14. Occlusal view (Fig 9) at 6 months postoperative.
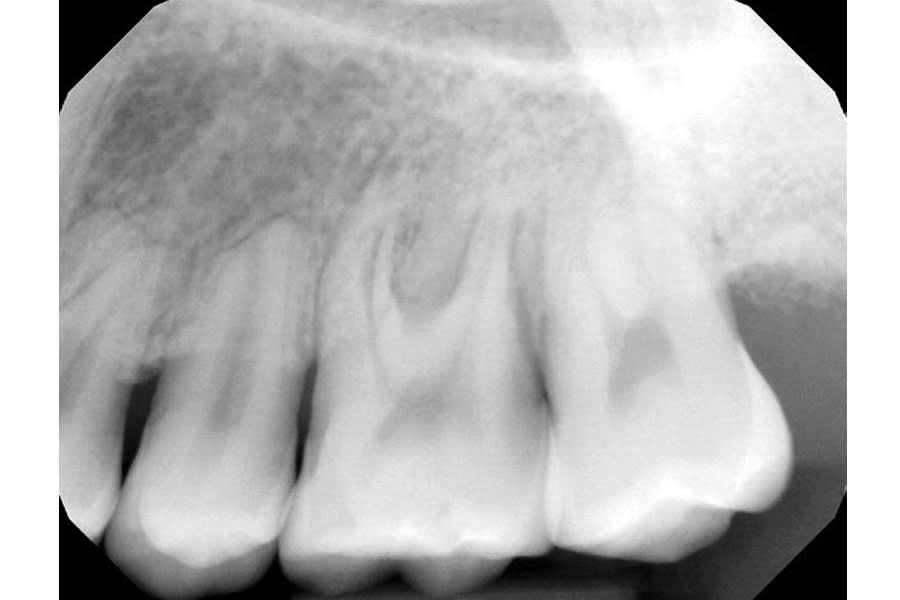
Figure 10
Fig 8 through Fig 11. Six-month periapical radiograph (Fig 10) and CBCT (Fig 11) imaging showing bone fill and improved density into the furcation at site No. 14.
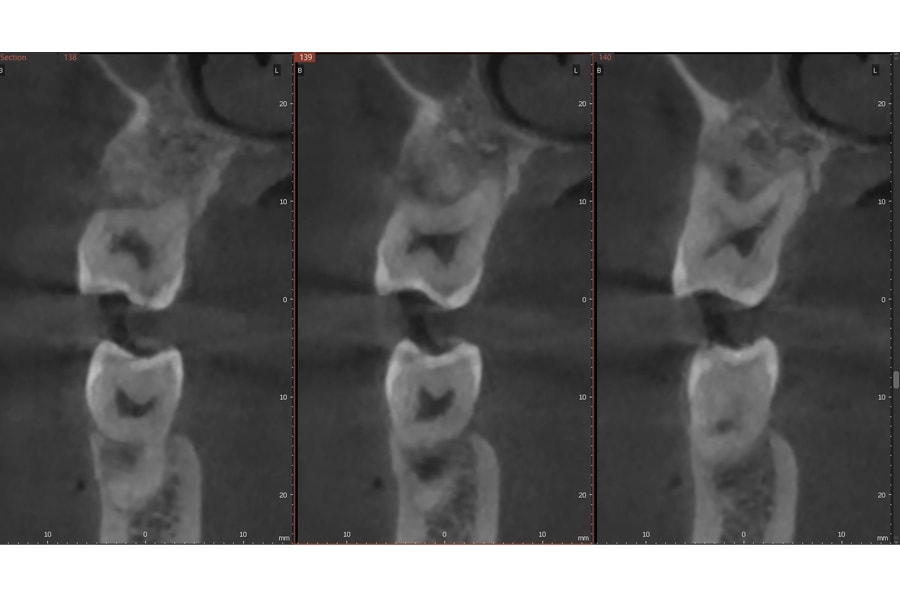
Figure 11
Fig 10 through Fig 11. Six-month periapical radiograph (Fig 10) and CBCT (Fig 11) imaging showing bone fill and improved density into the furcation at site No. 14.

Figure 12
Fig 12 through Fig 15. Twelve months after treatment. At 12 months postoperative (Fig 12), note improved tissue quality.

Figure 13
Fig 12 through Fig 15. Twelve months after treatment. At 12 months postoperative (Fig 12), note improved tissue quality. Occlusion continued to be evaluated at 6 and 12 months post-treatment, and adjustments were performed as needed (Fig 13).
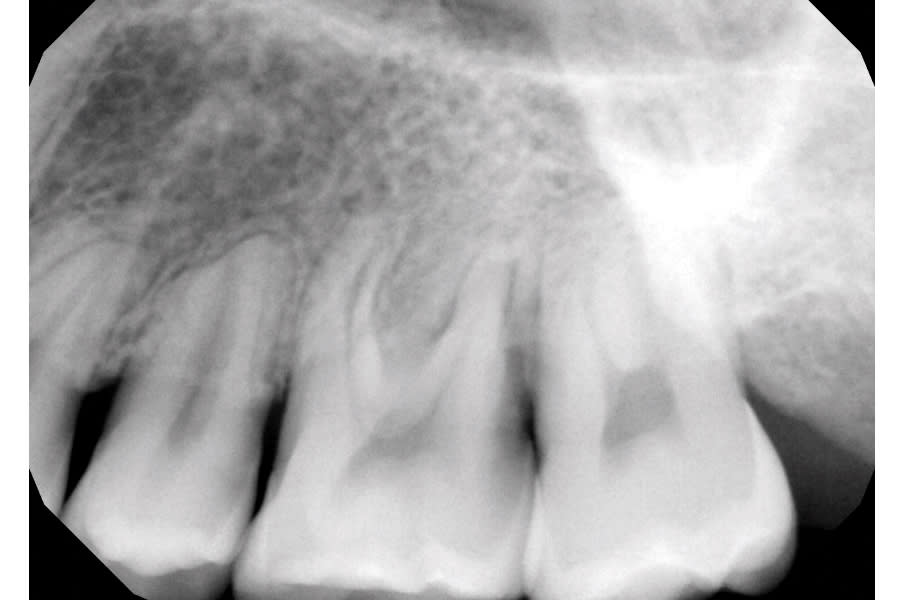
Figure 14
Fig 12 through Fig 15. Twelve months after treatment. At 12 months postoperative (Fig 12), note improved tissue quality. Occlusion continued to be evaluated at 6 and 12 months post-treatment, and adjustments were performed as needed (Fig 13). Periapical radiograph (Fig 14) and CBCT (Fig 15) imaging at 12 months post-treatment showing furcation bone regeneration at tooth No. 14 with continued bone density improvement.
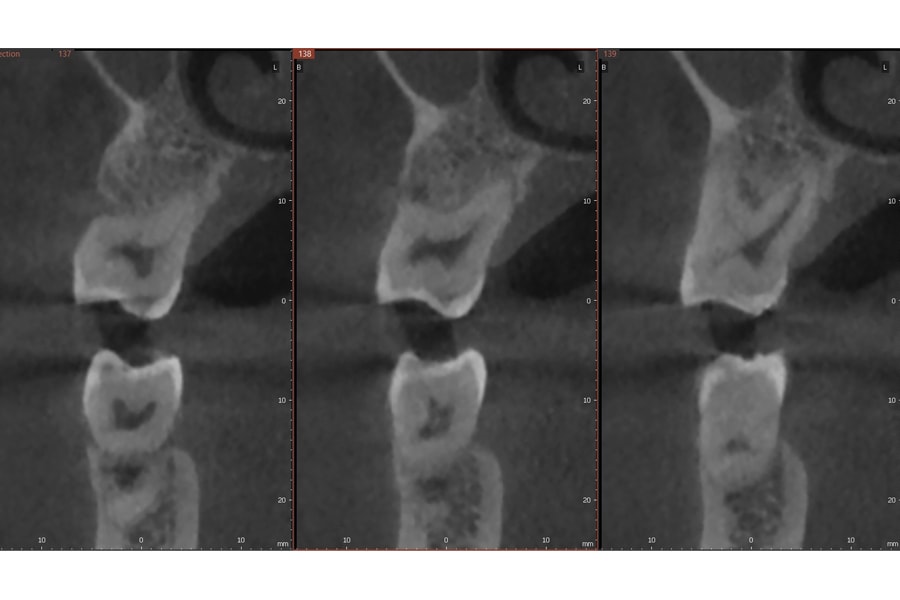
Figure 15
Fig 12 through Fig 15. Twelve months after treatment. At 12 months postoperative (Fig 12), note improved tissue quality. Occlusion continued to be evaluated at 6 and 12 months post-treatment, and adjustments were performed as needed (Fig 13). Periapical radiograph (Fig 14) and CBCT (Fig 15) imaging at 12 months post-treatment showing furcation bone regeneration at tooth No. 14 with continued bone density improvement. Clinical probing depth on the direct buccal of tooth No. 14 improved from 12 mm to 3 mm. Bone regeneration is expected to continue to improve for up to 3 years after LANAP treatment, with the majority of bone regeneration occurring within the first year.
