A 55-year-old male patient presented with advanced internal resorption of the upper right canine. The tooth was deemed nonrestorable and subsequently extracted in conjunction with alveolar ridge preservation, which was performed to attenuate post-extraction dimensional alteration. A zirconium-oxide resin-bonded fixed dental prosthesis (RBFDP) (Katana™ YML, Kuraray Noritake,
kuraraynoritake.com) was used as the long-term provisional prosthesis, bonded (CLEARFIL™ CERAMIC PRIMER PLUS, CLEARFIL™ Universal Bond Quick 2,
Panavia™ V5, Kuraray Noritake) to the first premolar. A single dental implant (BLX implant system, Straumann) was placed 4 months post-extraction in a two-stage approach with an immediate postoperative fixture-level intraoral scan done to facilitate a simultaneous implant-supported provisionalization upon fixture exposure. The provisional restoration was delivered immediately after second-stage surgery with a facial concavity to induce soft-tissue migration in the coronal direction. A conventional impression was taken, and shade information was recorded. The definitive implant-supported prosthesis was fabricated with a zirconium-oxide (Katana™ YML) framework and layered with feldspathic porcelain (Cerabien™ ZR, Kuraray Noritake) supported by a titanium base (Variobase®, Straumann). The prosthesis was designed with an emulated root form similar to the contralateral side and as appropriate for the surrounding periodontium.
KEY TAKEAWAYS
The use of modern ceramic technology allows for the fabrication of prostheses that closely replicate the appearance and function of natural teeth.
An FP2 prosthesis may serve as an alternative treatment option when soft-tissue augmentation is not indicated or pursued.
Dental photography and shade communication can help maximize clinical outcomes and aid in team collaboration.
Seung Jun Song, DMD, MS
Medical Staff, NewYork-Presbyterian Hospital, Columbia University; Assistant Professor in Dental Medicine, Columbia University, New York, New York
Sung Bin Im, MDC, CDT, BS
Chief Executive Officer, Sung Bin Im Dental Studio, Fort Lauderdale, Florida
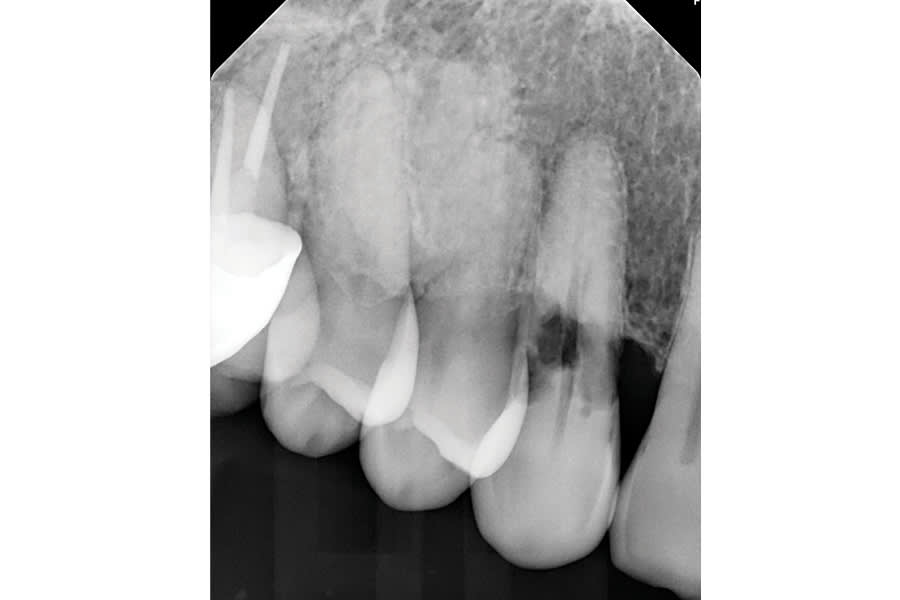
Figure 1
Fig 1. Preoperative periapical radiograph. Internal resorption of the upper right canine was observed, and the tooth was deemed nonrestorable.

Figure 2
Fig 2. RBFDP made in zirconium oxide with a single retainer design to engage the palatal aspect of the adjacent premolar.

Figure 3
Fig 3. Frontal view of the RBFDP.

Figure 4
Fig 4. Occlusal view of the RBFDP bonded to the premolar. The canine cusp was placed slightly buccal to avoid centric and excursive contact.

Figure 5
Fig 5. Frontal view of the upper right canine site at 4 months post-extraction.
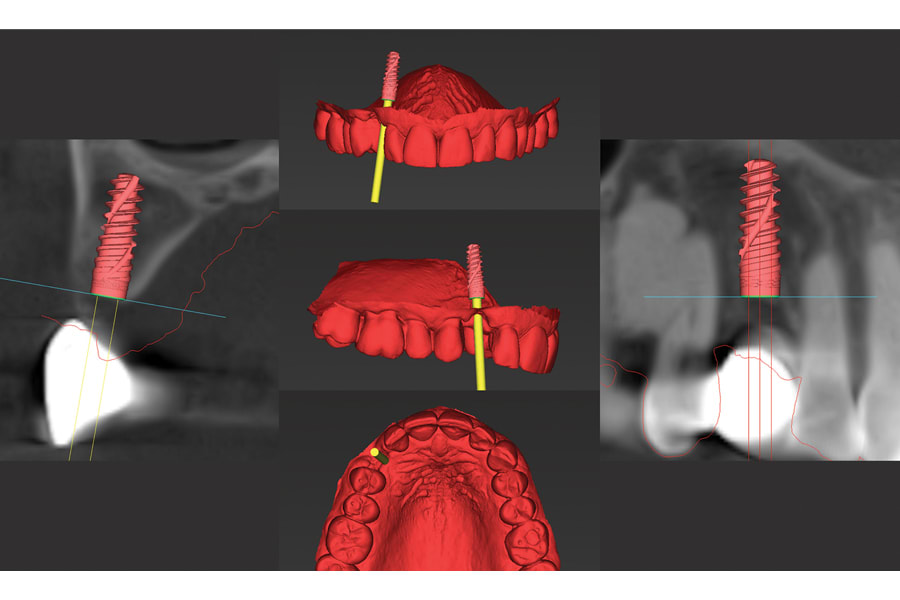
Figure 6
Fig 6. Various perspectives of the surgical plan for single implant placement at the upper right canine site.

Figure 7
Fig 7. A fixture-level intraoral scan was performed immediate postoperatively. The scan was utilized to fabricate an implant-supported provisional crown in preparation for second- stage surgery.

Figure 8
Fig 8. The implant-supported provisional crown was delivered immediately after second-stage surgery. The facial aspect had a concavity to induce vertical migration of the soft tissue.

Figure 9
Fig 9. Shade information was recorded with a standardized gray scale card and polarized filter.

Figure 10
Fig 10. Shade communication was reinforced with individual shade tabs.
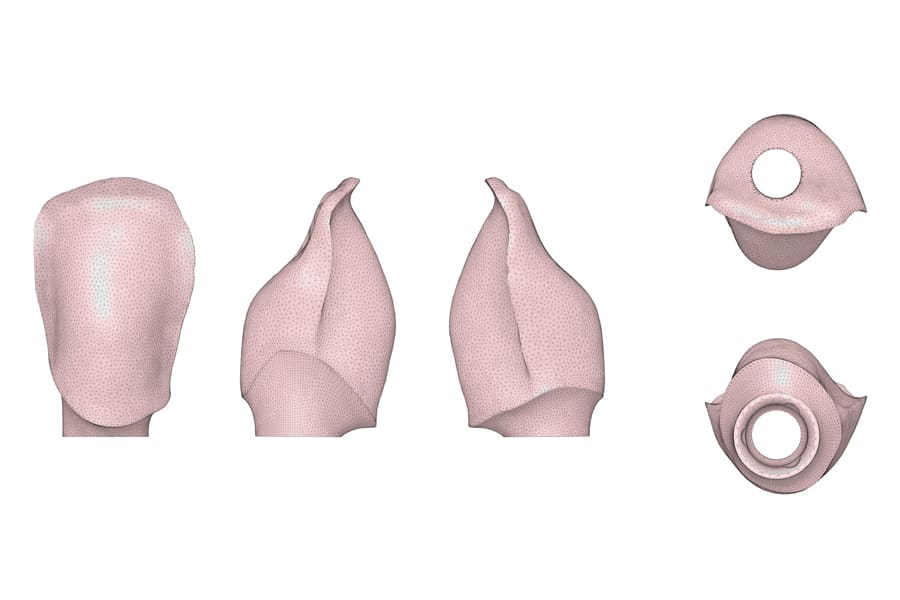
Figure 11
Fig 11. CAD rendering image of zirconium-oxide framework design for the implant-supported crown. The framework was designed to support the layered porcelain in the incisal and interproximal aspects.

Figure 12
Fig 12. Several views of the completed prosthesis with emulated root form design. The prosthesis is supported by a titanium base.

Figure 13
Fig 13 and Fig 14. The final prosthesis delivered; frontal view in maximum intercuspation position (Fig 13) and with contraster (Fig 14).

Figure 14
Fig 13 and Fig 14. The final prosthesis delivered; frontal view in maximum intercuspation position (Fig 13) and with contraster (Fig 14).

Figure 15
Fig 15. Post-delivery periapical radiograph.
